Australia’s aged care system is undergoing a significant transformation with the Support at Home Programme 2025, designed to deliver high-quality, person-centred care for older Australians. As part of our series exploring the Strengthened Aged Care Quality Standards (SAQS), this article focuses on Standard 6: Food and Nutrition. This standard acts like a “Best Practices” guide for food and nutrition, or a Manual for aged care diets. It guides residential aged care providers in delivering safe, nutritious, and enjoyable dining experiences that respect residents’ preferences and enhance their wellbeing, meeting aged care food standards.
What This Standard Means
Standard 6 mandates that older individuals in residential aged care receive nutritious, flavorful, and culturally appropriate meals. These are served in settings designed to foster joy and social connection. Providers must understand the diverse types of diets in aged care environments. To meet these aged care food standards, providers must collaborate closely with residents, customising dining experiences to align with individual preferences, needs, and cultural identities. This requirement applies exclusively to residential aged care services, ensuring each meal promotes both physical health and emotional well-being.
At the core of Standard 6 lies a commitment to respecting residents’ autonomy. Older Australians retain the right to choose their food, dining times, locations, and methods, including the option to exercise safe “dignity of risk.” This approach empowers them to shape their dining experiences, reflecting their unique values and personal identities.
Voices that matter:
- The elderly say: “I enjoy tasty and nutritious food every day.”
- The workers say: “I make sure our residents enjoy appetising and nutritious food every day.”
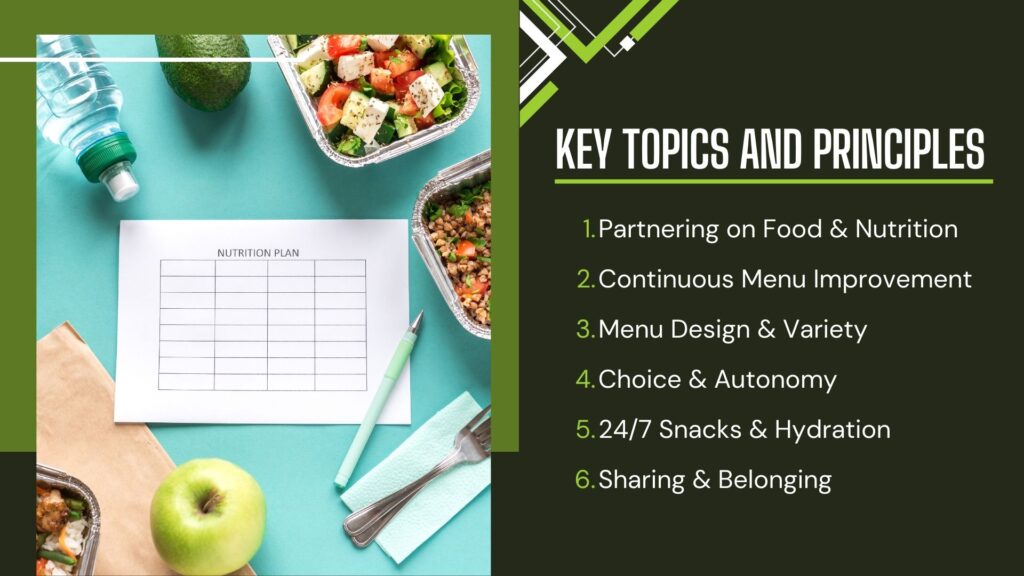
Key Topics and Principles
Standard 6 outlines key principles to make dining a highlight for residents:
- Partnering on Food & Nutrition: Co-design menus through resident feedback, tasting panels, and forums to reflect preferences. Why it matters: Collaboration ensures meals are personalised, boosting satisfaction and engagement.
- Continuous Menu Improvement: Dietitians regularly assess menus and mealtimes to ensure nutritional quality and variety. Why it matters: Ongoing evaluation keeps dining experiences relevant and health-focused.
- Menu Design & Variety: Menus are dietitian-approved, culturally safe, and include texture-modified options for diverse needs. Why it matters: Inclusive menus cater to all residents, respecting their cultural and health requirements.
- Choice & Autonomy: Flexible meal times and options allow residents to choose what, when, where, and how they eat. Why it matters: Autonomy fosters independence and dignity in dining.
- 24/7 Snacks & Hydration: Nutritious snacks and drinks, including water, are available at all times. Why it matters: Round-the-clock access supports hydration and nutrition, enhancing wellbeing.
- Sharing & Belonging: Dining spaces encourage residents to share meals with family and friends. Why it matters: Social dining strengthens community and emotional connections.
- Food Safety & Presentation: Meals are prepared safely, served at correct temperatures, and presented attractively, including moulded texture-modified foods. Why it matters: Safety and aesthetics build trust and elevate the dining experience.
Required Outcomes and Actions
Standard 6 is structured around 4 Outcomes and 10 Actions, with six actions introducing new expectations for providers. Two actions—regular menu and mealtime assessments (Action 6.2.1) and 24/7 access to snacks and drinks (Action 6.3.3)—are entirely new, while the others strengthen existing obligations. The outcomes and their corresponding actions are:
- 6.1 Partnering with Older People: Work with residents to shape food services and dining experiences that meet their preferences.
- Action 6.1.1: Partner with older people to understand their food and drink preferences, needs, and dining expectations.
- Action 6.1.2: Support older people to provide feedback about food, drink, and dining experiences and act on it to improve services.
- 6.2 Assessment of Nutritional Need and Preferences: Regularly assess nutrition, hydration, and dining preferences to adapt to changing needs.
- Action 6.2.1: Assess and regularly reassess each older person’s nutritional and hydration needs and dining preferences (new requirement).
- Action 6.2.2: Use assessments to inform food and drink preparation and dining experiences.
- 6.3 Provision of Food and Drink: Provide appetising, nutritious meals with ample choice and variety.
- Action 6.3.1: Provide food and drink that are safe, appetising, nutritious, and culturally appropriate.
- Action 6.3.2: Offer choice in food and drink, including when, where, and how it is served.
- Action 6.3.3: Ensure access to nutritious snacks and drinks, including water, at all times (new requirement).
- 6.4 Dining Experience: Create comfortable, social, and culturally safe mealtimes that foster belonging.
- Action 6.4.1: Provide dining experiences that are welcoming, comfortable, and culturally safe.
- Action 6.4.2: Support older people to dine with others, including family and friends, when they choose.
- Action 6.4.3: Ensure the dining environment promotes enjoyment, belonging, and connection.
These outcomes and actions ensure dining services are both functional and deeply enriching, supporting residents’ health and quality of life.
Demonstrating Conformance
To comply with Standard 6, providers must demonstrate robust systems and continuous improvement. Here’s how:
- Document Your Systems and Processes: Clearly document all processes to ensure consistent, accountable care delivery.
- Use Monitoring Tools for Improvement: Track staff adherence to processes and identify areas for enhancement.
- Collaborate with Care Recipients: Engage residents to gather insights and refine dining experiences based on their feedback.
- Observe Care Delivery in Action: Regularly observe meal preparation and service to identify strengths and opportunities.
- Gather and Use Feedback: Collect input from staff, managers, and governing bodies to drive quality improvements.
Reflective Questions for Providers
These questions help aged care providers assess how effectively they’re meeting the requirements of Standard 6:
- How do you ensure the key topics of Standard 6 are reflected in your dining experiences?
- How can you partner with older adults to create enjoyable and nutritious mealtimes?
- How do you gather feedback from residents and their allied health professionals about their food and dining needs?
How SAH Consulting Simplifies Support at Home Registration
Navigating Support at Home registration can be daunting, but SAH Consulting is your professional guide. Specialising in aged care compliance, we help residential providers meet the Strengthened Aged Care Quality Standards, including Standard 6, which is mandatory for Category 6 providers. Our services include gap-analysis audits, policy and procedure development, workforce-training frameworks, and end-to-end registration support.
With deep knowledge in food and nutrition compliance, SAH Consulting ensures your dining services meet regulatory expectations while delighting residents. Partner with SAH for stress-free registration and ongoing quality improvement, so you can focus on delivering exceptional care.
Final Thoughts
Standard 6: Food and Nutrition is an opportunity to transform dining into a nourishing, joyful, and dignified experience for older Australians. By prioritising choice, collaboration, and quality, providers can meet aged care food standards by creating mealtimes that residents cherish. Embracing Standard 6 not only ensures compliance but also positions you for success in delivering person-centred care.
Don’t wait to align with Standard 6. Partner with SAH Consulting to streamline your Support at Home registration and elevate your dining services. Act now to make every meal a moment of joy and connection!
